Wolff-Parkinson-White syndrome (WPW syndrome): различия между версиями
Wikiadmin (обсуждение | вклад) |
Wikiadmin (обсуждение | вклад) |
||
| Строка 11: | Строка 11: | ||
WPW syndrome can be detected at any age, even in newborns. Any concomitant heart disease, which proceeds with disorder of AV-conduction, can contribute to its manifestation. The persistent of the WPW syndrome, especially with arrhythmia attacks, disrupts intracardiac hemodynamics, which leads to a distension of the heart chambers and a decrease in the contractility of the myocardium. The course of the disease depends on the presence, frequency and duration of tachyarrhythmia. Sudden coronary death in WPW syndrome occurs in 4% of cases, usually due to fatal arrhythmias ([[atrial fibrillation]], [[atrial flutter]], ventricular tachycardia, [[ventricular fibrillation and ventricular flutter|ventricular fibrillation]]). | WPW syndrome can be detected at any age, even in newborns. Any concomitant heart disease, which proceeds with disorder of AV-conduction, can contribute to its manifestation. The persistent of the WPW syndrome, especially with arrhythmia attacks, disrupts intracardiac hemodynamics, which leads to a distension of the heart chambers and a decrease in the contractility of the myocardium. The course of the disease depends on the presence, frequency and duration of tachyarrhythmia. Sudden coronary death in WPW syndrome occurs in 4% of cases, usually due to fatal arrhythmias ([[atrial fibrillation]], [[atrial flutter]], ventricular tachycardia, [[ventricular fibrillation and ventricular flutter|ventricular fibrillation]]). | ||
| + | |||
| + | This pathology can be detected using ECG Dongle [https://cardio-cloud.ru/good/1] and ECG Dongle Full [https://cardio-cloud.ru/good/2]. | ||
Текущая версия на 12:31, 31 марта 2021
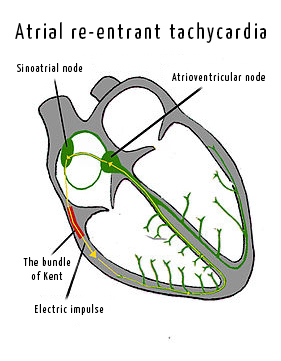
In this syndrome, the sinus impulse, after passing through the right Kent bundle (accessory pathway), activates part of the right ventricle earlier than the usual excitation of both ventricles occurs from the impulse that has come through the atrioventricular junction. Firstly, premature ventricular excitation, namely, part of the right ventricle (PQ interval is shortened), occurs. Secondly, a gradual, layer-by-layer activation of the right ventricular muscle mass occurs, which leads to the formation of a delta wave. Thirdly, not simultaneous excitation of both ventricles occurs: premature activation of the one part of the right ventricle, then all of it, then the interventricular septum and, finally, the left ventricle. Such a course of excitation of the ventricles resembles a left bundle branch block.
Some patients may not have clinical manifestations. The main manifestation of the Wolff-Parkinson-White syndrome is arrhythmia. In more than 50% of cases paroxysmal tachyarrhythmias occur: atrioventricular re-entrant tachycardia, atrial fibrillation, atrial flutter. Quite often, the syndrome occurs with heart disease: abnormality of Ebstein, hypertrophic cardiomyopathy, prolapse of the mitral valve.
There are several ways to treat the WPW syndrome:
- Antiarrhythmic therapy: constant intake of medications. Important: admission of Ca-blockers and digitalis preparations is unacceptable.
- Catheter ablation of the accessory pathway of conduction.
WPW syndrome can be detected at any age, even in newborns. Any concomitant heart disease, which proceeds with disorder of AV-conduction, can contribute to its manifestation. The persistent of the WPW syndrome, especially with arrhythmia attacks, disrupts intracardiac hemodynamics, which leads to a distension of the heart chambers and a decrease in the contractility of the myocardium. The course of the disease depends on the presence, frequency and duration of tachyarrhythmia. Sudden coronary death in WPW syndrome occurs in 4% of cases, usually due to fatal arrhythmias (atrial fibrillation, atrial flutter, ventricular tachycardia, ventricular fibrillation).
This pathology can be detected using ECG Dongle [1] and ECG Dongle Full [2].